“Can I Change My Health Plan Mid Year in Tampa Florida?”
According to recent statistics, approximately 62% of Americans receive their health insurance coverage through their employer. However, situations may arise where you may need or want to change your health plan mid-year. Tampa, Florida residents are no exception to this possibility. But is it actually possible to change your health plan mid-year in Tampa? Let’s explore this topic further.
Before we dive into the details, let’s clarify some definitions. A health plan is a contract between you and an insurance provider that states the medical and health care services you will receive and how much you will pay for them. Changing a health plan mid-year means altering your coverage, provider, or both before the annual enrollment period. The annual enrollment period typically occurs once a year, lasting for a limited duration.
The Annual Enrollment Period: Limitations on Changing Health Plans

The Annual Enrollment Period, or AEP, is the primary opportunity you have each year to make changes to your health plan. It typically takes place from October 15th to December 7th, with changes becoming effective on January 1st of the following year. During this time, individuals with Medicare can change their health plans, and employers offer open enrollment, allowing their employees to make changes to their health plans.
However, not everyone is bound by these limitations. There are certain circumstances where you may be eligible for a Special Enrollment Period (SEP), allowing you to change your health plan mid-year. It’s crucial to understand the specifics of these circumstances to determine if you qualify.
Losing Current Health Coverage
Losing your current health coverage is a common reason individuals may be eligible for a Special Enrollment Period. For instance, if you lose your job and, consequently, your employer-sponsored health insurance coverage, you may qualify for a SEP. This scenario includes being laid off, quitting your job, or having your hours reduced to the point where your eligibility for employer-sponsored coverage is revoked.
Other situations that may trigger a SEP due to the loss of current health coverage include:
– Losing coverage through a family member’s plan (e.g., due to divorce or death)
– Aging out of a parent’s plan (typically at the age of 26)
– Losing eligibility for Medicaid or the Children’s Health Insurance Program (CHIP)
Relocation and Coverage Availability
Get a hussle-free consultation
If you move to a new location, your options for health coverage may change. In certain cases, your current health plan may not be available in your new location, or you may have new options with your employer. Relocation triggers a Special Enrollment Period, allowing you to reassess your health insurance options.
However, it’s crucial to remember that moving within the same area does not typically qualify for a SEP. It would need to be a significant change in your physical residence, such as moving to a different ZIP code or county.
Eligibility for Medicaid or the Children’s Health Insurance Program
If you become eligible for Medicaid or the Children’s Health Insurance Program (CHIP) mid-year, you may qualify for a SEP. Both Medicaid and CHIP offer comprehensive health coverage options for low-income individuals and families. When your income or family situation changes, it’s essential to reassess your eligibility for these programs.
Exceptional Circumstances
In some cases, you may experience exceptional circumstances that impact your health insurance coverage. These could include divorce, marriage, or having or adopting a child. If you find yourself facing any of these scenarios, you may be eligible for a SEP and allowed to change your health plan mid-year.
It’s important to note that insurance providers and employers have different guidelines on what qualifies as exceptional circumstances. Therefore, it’s crucial to consult with your insurance provider to determine if your situation warrants a health plan change.
Health Insurance Experts at US Health Insurance Options LLC

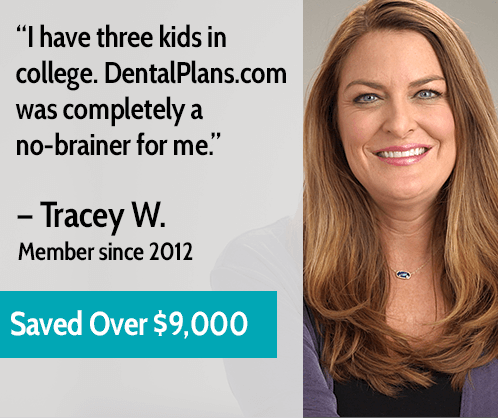
Changing your health plan mid-year can be a complex process. Understanding the eligibility criteria and navigating insurance options can quickly become overwhelming. This is where the health insurance experts at US Health Insurance Options LLC can offer their invaluable assistance.
Our team of professionals has extensive knowledge and experience in the health insurance industry, specifically in Tampa, Florida. We can help you determine if you qualify for a Special Enrollment Period and guide you through the process of changing your health plan mid-year. Whether you’re seeking individual coverage or need assistance with employer-sponsored options, our experts are here to ensure you make the best decision for your healthcare needs.
Contact our team today at (407) 588-0505 to speak with one of our friendly and knowledgeable representatives. Alternatively, you can fill out the quote request form on our website to request more information. We are here to help you navigate the intricacies of changing your health plan mid-year, ensuring you have the coverage you need.
Frequently Asked Questions
1. Can I change my health plan mid-year in Tampa, Florida?
Yes, you can change your health plan mid-year in Tampa, Florida if you qualify for a Special Enrollment Period (SEP). These special circumstances may include the loss of current health coverage, relocation, becoming eligible for Medicaid or CHIP, or experiencing exceptional life events.
2. What is the Annual Enrollment Period (AEP)?
The Annual Enrollment Period is the primary opportunity each year for individuals to make changes to their health plans. It usually lasts from October 15th to December 7th, with changes becoming effective on January 1st of the following year.
3. How do I know if I qualify for a Special Enrollment Period?
Qualification for a Special Enrollment Period depends on specific circumstances, such as losing current health coverage, relocating, becoming eligible for Medicaid or CHIP, or experiencing exceptional life events. It’s important to review the eligibility criteria and consult with your insurance provider to determine if you qualify.
4. What if I lose my job and my employer-sponsored health coverage?
If you lose your job and your employer-sponsored health coverage, you may qualify for a Special Enrollment Period. Losing current health coverage is a common trigger for a SEP, and you should explore your options during this time.
5. Can I change my health plan if I move within the same area?
Moving within the same area typically does not qualify for a Special Enrollment Period. You would need to experience a significant change in your physical residence, such as moving to a different ZIP code or county, to be eligible for a SEP.
6. What happens if I become eligible for Medicaid or CHIP mid-year?
If you become eligible for Medicaid or the Children’s Health Insurance Program (CHIP) mid-year, you may qualify for a Special Enrollment Period. These programs provide comprehensive health coverage for low-income individuals and families, and reassessing your eligibility is crucial.
7. Do exceptional life events qualify for a Special Enrollment Period?
Yes, exceptional life events such as divorce, marriage, or having or adopting a child may qualify for a Special Enrollment Period. However, insurance providers and employers may have different guidelines on what constitutes an exceptional circumstance, so it’s essential to consult with your insurance provider.
8. How can US Health Insurance Options LLC help me with changing my health plan mid-year?
US Health Insurance Options LLC can provide expert guidance and assistance in changing your health plan mid-year. Our knowledgeable professionals have extensive experience in the health insurance industry, specifically in Tampa, Florida. Contact us today at (407) 588-0505 or fill out our quote request form to learn how we can help.
9. Is consulting with health insurance experts necessary?
Consulting with health insurance experts at US Health Insurance Options LLC can significantly simplify the process of changing your health plan mid-year. Our experts have in-depth knowledge of the industry and can guide you through the eligibility criteria and available options, ensuring you make the best decision for your healthcare needs.
10. How can I contact US Health Insurance Options LLC for more information?
You can contact US Health Insurance Options LLC by calling (407) 588-0505 to speak with one of our representatives. Alternatively, you can fill out the quote request form on our website to request more information. We are here to provide you with the assistance you need to navigate the complexities of changing your health plan mid-year.
Consulting our health insurance experts at US Health Insurance Options LLC ensures you have the support and guidance necessary to make informed decisions about your health coverage. Call us at (407) 588-0505 or fill out the quote request form on this page to discover the benefits of relying on our expertise.

Resources
– Can I Change My Health Plan Mid Year in Tampa Florida
– Florida Medicaid
– Florida Medicare






0 Comments