How Long Do I Have To Change My Health Insurance?
When it comes to health insurance, timing is everything. Whether you’re switching providers, renewing your current plan, or purchasing coverage for the first time, understanding the timeline for making changes is crucial. But how long do you have to change your health insurance? In this comprehensive guide, we’ll explore the different scenarios and provide you with the information you need to make informed decisions about your health coverage.
“Health insurance is not a luxury; it is a necessity. Unfortunately, many Americans find themselves in a scramble when it comes to understanding the timeline for making important changes to their coverage.”
Changing Your Health Insurance during Open Enrollment
Can I change my health insurance plan during open enrollment?
Open enrollment is the period when you can make changes to your health insurance without needing a qualifying life event. In the United States, the open enrollment period typically runs from November 1 to December 15 for coverage starting the following year. During this time, you can switch plans, add or remove dependents, or enroll in coverage if you’re currently uninsured.
What happens if I miss the open enrollment period?
If you miss the open enrollment period, you’ll generally have to wait until the next enrollment period unless you experience a qualifying life event. However, certain states may have additional or extended open enrollment periods, so it’s important to check with your state’s health insurance marketplace or consult with a licensed insurance agent to explore your options.
Special Enrollment Period (SEP)
What is a special enrollment period?
A special enrollment period (SEP) is a time outside the regular open enrollment period when you can still enroll in or make changes to your health insurance plan. It is triggered by qualifying life events such as getting married, having a baby, losing other health coverage, or moving to a new state.
How long do I have to change my health insurance plan during a special enrollment period?
The length of a special enrollment period varies depending on the qualifying life event. For example, if you lose your job-based coverage, you generally have 60 days from the date of job loss to enroll in a new plan. If you experience another qualifying life event, such as getting married or having a child, you typically have 60 days from the event to make changes to your coverage. It’s important to act promptly during a special enrollment period to ensure you don’t miss the deadline.
Off-Exchange Plans and Individual Health Insurance
Get a hussle-free consultation
Can I change my off-exchange health insurance plan any time?
If you have an off-exchange individual health insurance plan, you may have more flexibility in changing your coverage outside of the regular open enrollment period. However, it’s important to note that individual health insurance plans may have specific enrollment periods or restrictions, so it’s crucial to check with your insurance provider or a licensed insurance agent for the most accurate information.
What are the key differences between on-exchange and off-exchange health insurance plans?
On-exchange health insurance plans are purchased through the health insurance marketplace and may be eligible for premium subsidies and cost-sharing reductions based on your income. Off-exchange plans, on the other hand, are purchased directly from an insurance company and do not qualify for subsidies. The choice between the two options depends on your unique circumstances, financial situation, and coverage needs.
Medicare and Medicaid
Can I change my Medicare plan at any time?
Medicare recipients have specific enrollment periods to make changes to their plans. The Annual Enrollment Period (AEP) for Medicare Advantage and Medicare prescription drug coverage runs from October 15 to December 7 each year. During this period, you can switch Medicare Advantage plans, join a Medicare Advantage plan, switch or join a Medicare prescription drug plan, or return to Original Medicare. There are also special enrollment periods for certain circumstances, such as moving to a new area or losing other coverage.
How long do I have to make changes to my Medicaid plan?
Medicaid recipients may be able to make changes to their plans at any time, as Medicaid operates on a continuous open enrollment model. However, certain states may have specific rules or enrollment periods, so it’s important to check with your state’s Medicaid program for detailed information.
Cobra Coverage and Job Loss
What is COBRA coverage?
COBRA (Consolidated Omnibus Budget Reconciliation Act) is a federal law that allows employees to continue their employer-sponsored health insurance coverage for a limited period of time after leaving a job or experiencing a reduction in work hours. COBRA coverage can bridge the gap in your health insurance during such transitions.
How long do I have to enroll in COBRA coverage?
Typically, employees who qualify for COBRA have 60 days from the date of job loss or qualifying event to elect coverage. Once you elect coverage, you generally have 45 days to submit the initial premium payment. It’s essential to act promptly to avoid coverage gaps and potential penalties.
In conclusion, the timeline for making changes to your health insurance varies depending on various factors, including open enrollment periods, qualifying life events, the type of coverage you have, and specific state rules. Understanding these timelines and staying proactive can help ensure you have the coverage you need when you need it.
Frequently Asked Questions
- Can I change my health insurance plan outside of open enrollment?
- How can I determine if I qualify for a special enrollment period?
- What should I do if I miss the open enrollment period and don’t have a qualifying life event?
- Can I change my off-exchange health insurance plan at any time?
- How often can I make changes to my Medicare plan?
- What should I do if I lose my job and need health insurance coverage?
- Can I make changes to my Medicaid plan at any time?
- What happens if I miss the deadline to enroll in COBRA coverage?
- How can I get more information about changing my health insurance?
- Why should I consult health insurance experts at US Health Insurance Options LLC?
Yes, you may be able to change your health insurance plan outside of open enrollment if you experience a qualifying life event, such as marriage, having a baby, or losing other coverage.
You can determine if you qualify for a special enrollment period by reviewing the list of qualifying life events provided by your health insurance marketplace or consulting with a licensed insurance agent.
If you miss the open enrollment period and don’t have a qualifying life event, you may have to wait until the next enrollment period. However, some states have additional or extended open enrollment periods, so it’s important to check with your state’s health insurance marketplace.
Off-exchange health insurance plans may have specific enrollment periods or restrictions, so it’s crucial to check with your insurance provider or a licensed insurance agent for the most accurate information.
Medicare recipients can make changes to their plans during the Annual Enrollment Period (AEP) from October 15 to December 7 each year, as well as during special enrollment periods for certain circumstances.
If you lose your job and need health insurance coverage, you may be eligible for COBRA coverage or may qualify for a special enrollment period to enroll in an individual health insurance plan.
Medicaid operates on a continuous open enrollment model, but specific rules or enrollment periods may vary by state, so it’s important to check with your state’s Medicaid program for details.
If you miss the deadline to enroll in COBRA coverage, you may lose the opportunity to continue your employer-sponsored health insurance and might have to explore other coverage options.
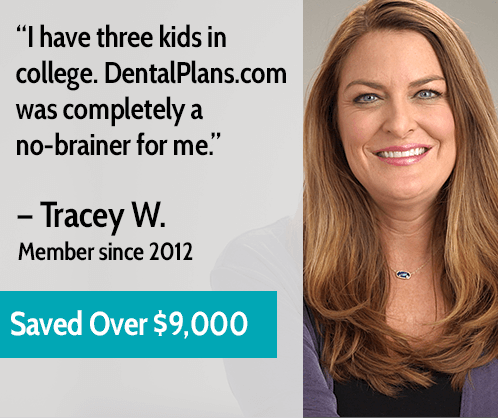
US Health Insurance Options LLC has a team of health insurance experts who can provide personalized guidance and assist you in navigating the complexities of changing your health insurance. Call (407) 588-0505 or fill out the quote request form on this page to get started.
Our health insurance experts have in-depth knowledge of the industry, a vast network of insurance providers, and a commitment to helping individuals and families find the best coverage options for their unique needs. We will guide you through the process, answer your questions, and ensure you have the peace of mind that comes with having the right health insurance.
Choosing the right health insurance is essential for your well-being and financial security. Take advantage of the expertise and support provided by our team at US Health Insurance Options LLC. Call (407) 588-0505 or request more information by filling out the quote request form on this page. We’re here to help you make informed choices and find the health insurance coverage that fits your needs.







0 Comments